Urology vs. NephrologyBy: Kayla Holmes
Nephrology and Urology work hand in hand to treat the kidneys and urological system. There is often overlap in what organs and systems are involved in these specialities. So what’s the difference? How do I know which I need to see? Read below to learn more about how these two specialties come together to create a dynamic duo for kidney health. Urology According to the Urological Care Foundation, “Urology is a part of health care that deals with diseases of the male and female urinary tract (kidneys, ureters, bladder, and urethra). It also deals with the male [reproductive] organs... Since health problems in these body parts can happen to everyone, urologic health is important.” Common conditions that urologists treat are:
Nephrology Nephrology is a branch of medicine that treats the kidneys. This can include the treatment of kidney diseases, monitoring kidney function, maintaining kidney health, and beginning renal replacement therapies. Common conditions that nephrologists treat are:
How do they work together? Urology and nephrology each treat different sides of the same coin. Kidney stones are a great example of how these two specialties work together. Nephrology will treat the prevention of stones through assessing lab work and imaging studies and suggesting changes to the diet or medication regimen. Urology will perform the necessary procedures to remove the stones if/when they become an issue. Who do I need to see? If you are experiencing frequent urinary tract infections, kidney stones, kidney cysts, or other conditions that involve the urinary and renal systems, urology is usually your best option. However, if you feel you need to see a nephrologist and are concerned about your kidney function, we are more than happy to see you and evaluate your needs. Munjal’s Musings: Urologists are the surgeons who deal with the hardware, removing the bad parts and making repairs. Nephrologists are medical doctors that will handle the software, making sure the kidneys are filtering and functioning properly. Resources: https://www.urologyhealth.org/urology-a-z/what-is-urology By: Kayla Holmes 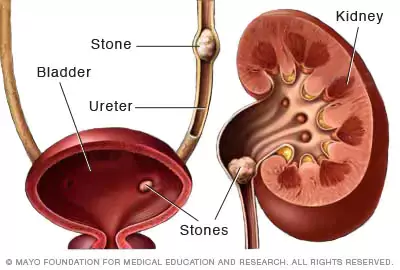 Kidney stones can be a frightening diagnosis to hear. These are often regarded as painful, uncomfortable, irritating, and scary. The possibility of passing it naturally or going through surgery can cause a great deal of stress. Let’s discuss what kidney stones are, the signs to look for, and how we can help you get the care you need. What are kidney stones? According to the Mayo Clinic, “kidney stones (also called renal calculi, nephrolithiasis or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys.” Kidney stones can be caused by a wide range of things like medications and supplements, diet, certain chronic illnesses, and body weight. How can I tell if I have a kidney stone? Some kidney stones can be passed without the patient even knowing. However, when there is a stone too large to pass or a significant build up of salts and minerals, there may be signs that you need to see a specialist.
Who do I need to see and what are my next steps? You will want to call a urologist as soon as possible. There are various labs or imaging that can be ordered. If the pain and discomfort is too intense, visit your closest emergency room or urgent care for evaluation. After seeing urology, they may refer you to a nephrologist to discuss the cause and prevention methods. If you suspect you may have a kidney stone, seek medical help as soon as possible. Nephrologists and urologists are here to help find the cause and treat the symptoms. As always, stay safe and healthy. Resources: https://www.mayoclinic.org/diseases-conditions/kidney-stones/symptoms-causes/syc-20355755 This website is for informational and educational purposes ONLY. While we strive for accurate, general medical information, this does not replace professional medical advice. Do not rely solely on this information. Please consult with your physician for more information regarding your specific needs. If you are experiencing a medical emergency, please call 911. How Much is Too Much?In our last segment of the Kidney Korner, we discussed what fluids are and foods that have high water content, or insensible fluids (read about it here). This month, we are discussing hydration and how much fluid is too much for the kidneys to handle.
If you drink too much fluid, your kidneys may not be able to process and filter it properly (especially if you have kidney diseases) causing a myriad of problems. Decreased kidney function, Congestive Heart Failure (CHF), edema, liver diseases, and muscular issues have been linked to fluid retention. It is extremely important to maintain the balance of fluids and electrolytes in your body to stay healthy. Symptoms of overhydration can include swelling, increased trips to the bathroom (see the exceptions below), and clear, colorless urine (looks like water). There are many exceptions and special circumstances to consider when it comes to fluid intake.
Munjal’s Musings: How often do you water your plants? It can be complicated. You have to ask a few questions:
The same goes for people. Size, health status, medications, occupation, location, and the season are just a few of the elements that go into determining proper fluid intake for a person. You can also view hydration like filling a bucket. You want the bucket to be nicely topped off, not overflowing or only half full. It is a balancing act. It is important to have routine lab work done regularly and discuss your individual needs with your doctor(s). There is no universal guideline for the amount of fluids a person should consume daily. Tune in next week as we continue our segment on fluids and discuss the symptoms of dehydration and when to seek help. This website is for informational and educational purposes ONLY. While we strive for accurate, general medical information, this does not replace professional medical advice. Do not rely solely on this information. Please consult with your physician for more information regarding your specific needs. If you are experiencing a medical emergency, please call 911. When a patient gets diagnosed with Chronic Kidney Disease, a lot of questions about diet and fluid intake tend to come up. How much should I drink? What should I eat? What needs to be taken out or altered in my normal diet? These can be daunting and seem overwhelming. An easy switch can be to reduce the added salt, or sodium chloride, when cooking. Added salt can come from your table salt shaker or other seasoning mixes commonly found in your spice cabinets. Added sodium can also come in the form of preservatives in canned goods, frozen foods, and boxed meals or ingredients. For more information on sodium, you can review our Kidney Korner segment on sodium here.
Common Seasonings with Added Salt
Seasonings as Salt Replacements
Be sure to check the labels of your spice bottles in all circumstances to ensure that it is truly free of sodium. When they have phrases like “No Salt Added,” “Salt Free,” and “Low Sodium,” it can mean that the salt has been replaced with potassium chloride, a different version of salt. This can be just as problematic as sodium chloride for patients with kidney diseases and hypertension. You can learn more about how to cook and season your food with spices instead of salt from the National Kidney Foundation here. If you have any questions or concerns about salt and sodium in your diet, you can contact your care team for additional assistance. As always, stay safe and healthy! Resources: https://www.nhlbi.nih.gov/health/educational/healthdisp/pdf/tipsheets/Use-Herbs-and-Spices-Instead-of-Salt.pdf Hurricane season (June 1- November 30, 2023) is upon us. It’s important to be prepared if or when disaster strikes. More information and advice for preparing for hurricane season can be found here:
https://www.floridadisaster.org/planprepare/preparing-for-hurricane-season/ https://www.ready.gov/ https://www.cdc.gov/disasters/hurricanes/index.html Tax Free: May 27- June 09, 2023 August 26- September 08, 2023 https://floridarevenue.com/taxes/tips/Documents/TIP_23A01-02.pdf In addition to basic food and household supplies, it is important to have an emergency supply of prescription medications. We recommend that there is at least 2 to 3 weeks worth of medications on hand in an emergency preparedness kit. A great way to store these are with pill bags or resealable plastic bags. The prescription name, dosage, frequency, and expiration date can be written on the front of the bag for ease of identification. Please contact your pharmacy for timely refills of your medications. For those who may want or need to evacuate or do not feel comfortable traveling to our office, we will be continuing to offer virtual visits. Virtual visit coverage for Medicare patients has been extended to December 31, 2024. For commercial insurance, please contact your insurance carrier to inquire about virtual visit coverage under your plan’s contract. This is subject to change as more information is released. As always, stay safe and healthy! References: Florida Dept. of Revenue - Home. Florida Department of Revenue. (n.d.). Retrieved June 6, 2022, from https://floridarevenue.com/DisasterPrep/Pages/default.aspx Home. FloridaDisaster.org. (n.d.). Retrieved June 6, 2022, from https://www.floridadisaster.org/ https://www.flsenate.gov/Media/PressRelease/Show/4446#:~:text=The%20legislation%20creates%20a%2014,2023%2C%20for%20disaster%20preparedness%20supplies. |
About The BeanThe Bean is a blog on a mission to share valuable information in the world of Nephrology. We believe in empowering through education and The Bean is a great place to find resources and information on topics related to high blood pressure, kidney disease, dialysis, and topics that enhance the kidney minded lifestyle. Enjoy and be sure to subscribe! Archives
July 2024
Categories |
Contact Us |
Careers |
Connect With Us |
|
13241 Bartram Park Blvd., Suite 1001
Jacksonville, FL 32258 Open Map Tel: (904) 260-9898 Fax: (904) 260-9891 |
Interested in joining our team? Jacksonville Nephrology is dedicated to compassionate patient care through teaching and giving our team the tools needed to go above and beyond. Learn more about current openings. Learn More
|